Medicaid Cuts and ACA Changes Hit Non-Expansion States Hard
New federal budget law containing Medicaid funding cuts and ACA changes disproportionately impact Medicaid non-expansion states, increasing uninsured numbers and straining rural hospitals.
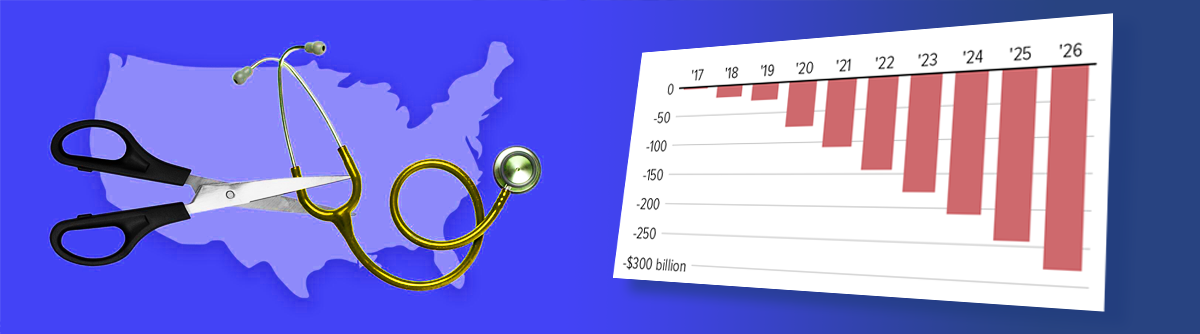
New federal budget law containing Medicaid funding cuts and ACA changes disproportionately impact Medicaid non-expansion states, increasing uninsured numbers and straining rural hospitals.
Congress debates the future of Affordable Care Act subsidies and Medicaid expansion, impacting health insurance affordability and healthcare access across many states.
Exploring the Affordable Care Act's comprehensive approach to reducing racial health disparities and the political opposition shaping U.S. healthcare policy.
CMS releases preliminary guidance for states to implement Medicaid community engagement requirements by 2027, detailing eligibility, exemptions, verification, and compliance procedures.
Court ruling confirms Congressional power to enact health care reform, supporting Medicaid expansion and anti-discrimination insurance protections in California and nationwide.
Explore how new federal legislation will raise health insurance premiums, expand Medicaid work requirements, and affect healthcare funding in North Carolina starting in 2026.
The 2025 Commonwealth Fund Medicare Scorecard ranks Gulf South states lowest nationally due to challenges in access, quality, costs, and population health for older adults and disabled Medicare beneficiaries.
Federal court pauses ACA eligibility changes while Supreme Court blocks NIH grant restorations, impacting healthcare policy and funding. Explore implications for insurance and Medicaid expansion.
Analysis shows Trump-era policies and tax credit expirations will significantly raise ACA marketplace premiums, disproportionately impacting rural residents in 32 states.
Explore the implications of the 2025 One Big Beautiful Bill Act on Medicare and Medicaid programs, focusing on coverage changes, eligibility hurdles, and the impact on rural hospitals and long-term care.