Medicaid Cuts and ACA Changes Hit Non-Expansion States Hard
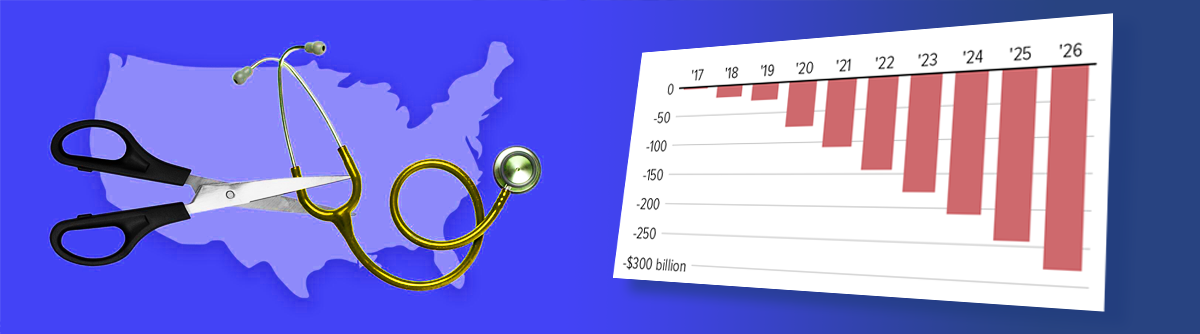
The recently enacted Republican budget law containing several priorities from former President Donald Trump has significant implications for Medicaid expansion holdout states. These 10 states, which have not expanded Medicaid under the Affordable Care Act (ACA), are expected to experience considerable burdens similar to those in the 40 states that expanded Medicaid. One major effect includes an increase in uninsured individuals due to cuts in Medicaid funding exceeding $1 trillion over the next decade and restrictions that tighten enrollment procedures for ACA marketplace plans. Georgia, with a population of approximately 11 million, is projected to lose as many ACA marketplace enrollees as California, which has over three times its population, highlighting disproportionate impacts on non-expansion states.
if enhanced ACA subsidies are not extended, "everyone will be hit hard", but non-expansion states will see a larger share of residents reliant on the marketplace, particularly those at lower income levels.
— Cindy Mann Health Expert
The budget law reduces federally funded navigators’ support and shortens enrollment periods, measures that will notably reduce ACA plan enrollments, especially in states with higher reliance on these plans such as Florida and Texas. The Congressional Budget Office estimates that 10 million people will lose coverage over the next decade due to the law's provisions. Enhanced ACA subsidies critical to keeping premiums affordable may expire at the end of the year, potentially causing premiums to increase by over 75%, threatening to push millions more in non-expansion states, like Florida, into uninsured status.
Hospital and health policy experts point out that the states which opted to expand Medicaid have generally seen more favorable outcomes and financial stability compared to non-expansion states facing similar fiscal pressures without the advantage of expanded federal support. Non-expansion states typically spend less per Medicaid enrollee and provide fewer medical benefits while covering fewer low-income Americans.
Additional challenges for non-expansion states include cuts starting in 2028 to directed payments—state financing arrangements used to increase Medicaid reimbursements—which will be reduced incrementally to levels closer to Medicare payments. These cuts threaten rural hospitals which rely on higher Medicaid reimbursements to remain operational. A $50 billion federal fund aims to mitigate some rural healthcare losses but covers only a portion of the anticipated cuts.
Non-expansion states also received extended uncompensated care pool financing programs during the previous administration, which support hospitals treating uninsured patients but do not provide health coverage or preventive care to individuals. This financing strategy contrasts with Medicaid expansion’s objective of increasing insured populations.
Public health leaders express concerns about deteriorating healthcare access in non-expansion states; issues include insufficient Medicaid coverage for vulnerable groups like children, older adults, and people with disabilities, contributing to hospital closures and reduced access to specialized care. This may lead to greater reliance on emergency care and increased long-term state healthcare expenditures.
State officials from non-expansion states have not indicated shifts toward Medicaid expansion despite the growing financial and healthcare pressures exacerbated by the new budget law. At the same time, there is skepticism about state governments’ ability or willingness to compensate for federal funding reductions.
Insurance markets in non-expansion states are vulnerable to collapse due to rising uninsured rates and reduced market participation from insurers. Experts warn that the expiration of enhanced ACA subsidies could accelerate this trend, undermining market stability and patient access.
This legislative environment highlights ongoing disparities between Medicaid expansion and non-expansion states, particularly regarding coverage accessibility, healthcare outcomes, and financial sustainability for providers and patients alike. The law’s long-term impact will depend on potential future policy changes, including renewal of ACA subsidies and any state decisions to pursue Medicaid expansion.
Health policy analysts and hospital leadership emphasize the complex fiscal and care access challenges facing the healthcare systems in non-expansion states due to the confluence of Medicaid cuts, marketplace enrollment declines, and limited state-level responses. These factors combine to heighten the risks of negative healthcare outcomes and financial instability within affected states.
In summary, the new Medicaid funding reductions and ACA marketplace enrollment restrictions embedded in the Republican budget law will disproportionately affect non-expansion states. They face both immediate and long-term challenges related to insurance coverage losses, increased uninsured populations, provider reimbursement cuts, and constrained access to comprehensive care services. These impacts underscore the ongoing divide in health policy outcomes among states based on Medicaid expansion decisions.