CMS Launches MAHA ELEVATE Model to Advance Functional and Lifestyle Medicine in Medicare
CMS Signals a Broader View of Value Based Care With MAHA ELEVATE
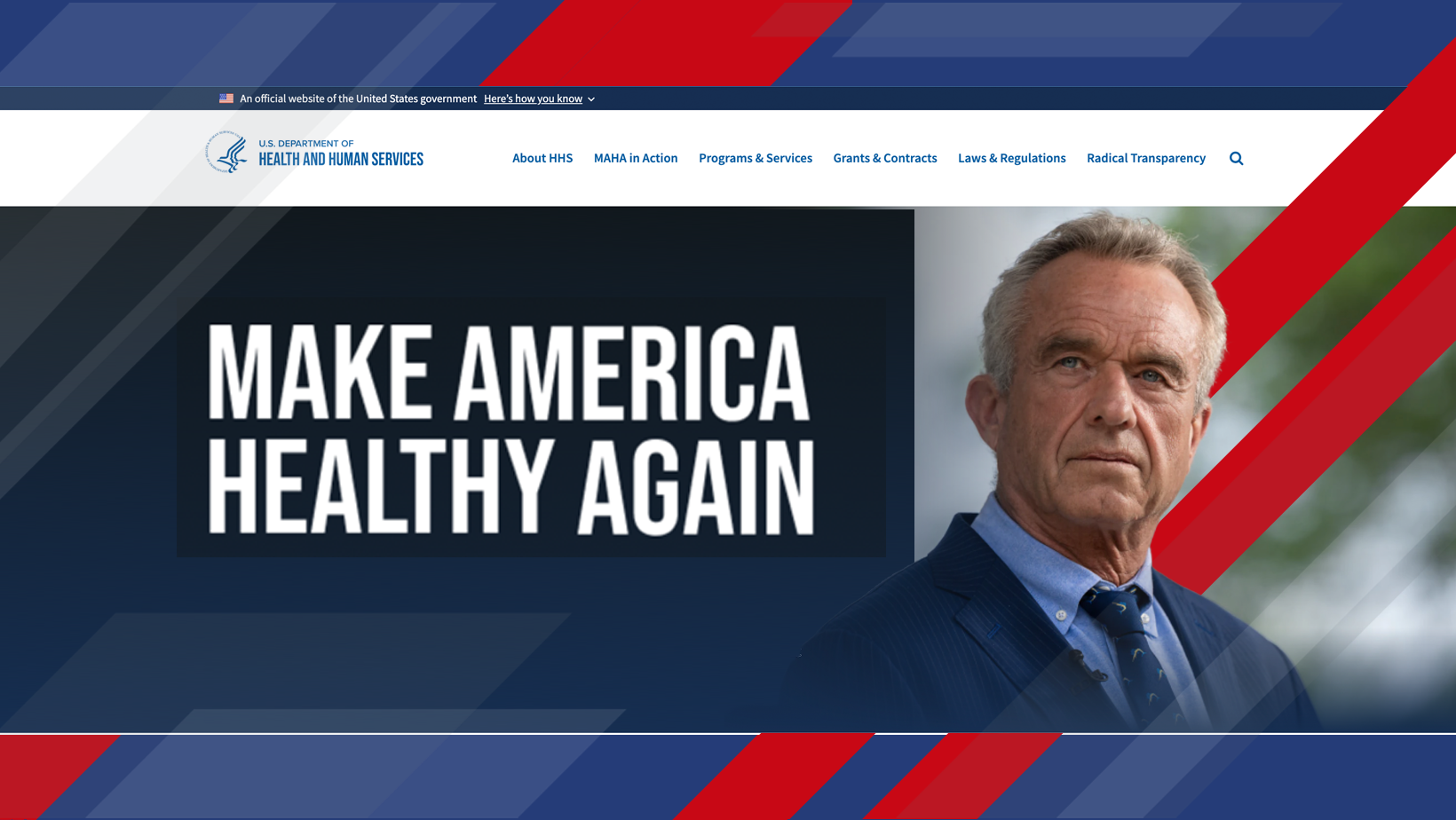
The Centers for Medicare and Medicaid Services is continuing its steady expansion of what value based care can look like in practice. With the launch of the Make America Healthy Again: Enhancing Lifestyle and Evaluating Value-based Approaches Through Evidence model, better known as MAHA ELEVATE, CMS is testing whether functional and lifestyle medicine can play a measurable role in improving outcomes for Medicare beneficiaries.
For insurers, provider groups, and care management organizations, the model offers an early look at how federal policy is beginning to treat prevention, nutrition, and whole person care not as add ons, but as core strategies tied to cost control and quality.
What MAHA ELEVATE Is Designed to Do
MAHA ELEVATE is structured as a three year initiative backed by roughly $100 million in funding. CMS plans to support up to 30 cooperative agreements with organizations that have experience delivering and evaluating integrative care models alongside traditional Medicare services.
The focus is clear. CMS wants evidence that lifestyle driven interventions can slow disease progression, improve quality of life, and do so without raising costs for beneficiaries.
“This model reflects CMS’s growing interest in approaches that address root causes of chronic disease while remaining accountable for outcomes and spending.”
CMS Innovation Center spokesperson
The program places particular emphasis on dementia care, an area where quality of life, caregiver burden, and long term costs intersect sharply. By funding models that blend nutrition, physical activity, behavioral health, and conventional treatment, CMS is signaling that chronic disease management is not limited to clinical encounters alone.
Why This Matters to the Insurance Industry
For health plans and risk bearing organizations, MAHA ELEVATE reinforces several trends already underway.
Key implications to watch
-
A broader definition of covered value based activities that extends beyond traditional clinical services.
-
Increased emphasis on prevention and lifestyle interventions as cost containment tools.
-
New evaluation frameworks that may influence future coverage and reimbursement decisions.
Insurers that operate Medicare Advantage plans or partner closely with accountable care organizations will want to pay close attention to how CMS measures success under this model. If outcomes show promise, similar approaches could eventually influence benefit design, supplemental offerings, and care management strategies.
Alignment With the Next Generation of CMS Models
MAHA ELEVATE does not stand alone. It fits into a larger pipeline of Innovation Center activity, including the planned Advancing Chronic Care with Effective, Scalable Solutions model scheduled to launch in 2026. ACCESS is expected to lean heavily on technology enabled care and scalable solutions for chronic disease management.
Together, these models illustrate a dual strategy. CMS is exploring both high tech and high touch approaches, testing digital tools on one hand and lifestyle focused care on the other.
“We see MAHA ELEVATE as complementary to where Medicare is headed, especially as organizations look for new pathways beyond existing ACO models.”
NAACOS leadership
This is particularly relevant as ACO REACH phases out and accountable care organizations search for new frameworks that preserve flexibility while maintaining financial accountability.
A Shift Toward Holistic Value Measurement
At its core, MAHA ELEVATE reflects a philosophical shift. CMS is increasingly open to measuring value through patient experience, functional outcomes, and long term health trajectories rather than relying solely on utilization metrics.
For insurers, that shift raises important questions. How do you price prevention? How do you evaluate returns that accrue over years rather than quarters? And how do you integrate nontraditional care partners into regulated payment models?
A simplified view of the evolution looks like this:
| Medicare Model Direction | Primary Focus |
|---|---|
| Early value based models | Utilization and cost reduction |
| Current generation | Quality metrics and care coordination |
| Emerging models | Prevention, lifestyle, and whole person outcomes |
Looking Ahead
MAHA ELEVATE is still a pilot, but its existence speaks volumes. CMS is clearly willing to experiment with diversified care delivery methods that move upstream, closer to the drivers of chronic disease. For the insurance industry, this is less about a single model and more about preparing for a future where value based care encompasses nutrition, behavior, and daily living as much as procedures and prescriptions.
The organizations that succeed will be those that can translate these broader definitions of health into measurable outcomes and sustainable financial performance.
