Freedom Health Settles Medicare Advantage False Claims for $31.7M
Freedom Health’s $31.7M Medicare Advantage Settlement: A Wake-Up Call for the Industry
The insurance industry has once again been reminded that compliance is not optional. Freedom Health Inc., a Tampa-based managed care provider, recently agreed to pay $31.7 million to resolve allegations of violating the False Claims Act. At the heart of the case were accusations that the company engaged in schemes to inflate Medicare Advantage payments, ultimately costing the government—and taxpayers—millions.
Adding to the fallout, former Chief Operating Officer Siddhartha Pagidipati will personally pay $750,000 for his role in the misconduct. This dual accountability underscores regulators’ focus on both corporate and individual responsibility.
Why This Matters for Insurers
Medicare Advantage plans have been under heightened scrutiny for years, but this settlement signals that oversight is entering a more aggressive phase. Federal regulators and enforcement agencies are increasingly willing to pursue cases that hinge on improper coding, inflated risk scores, or questionable reporting practices.
“The government is sending a clear message: companies and executives cannot game the system without consequences.”
— Health Care Compliance Analyst
For insurers, this isn’t just about one company’s missteps—it’s about the broader message of accountability in an era of tightening enforcement.
Key Takeaways for the Insurance Industry
Here are a few of the most important lessons insurers should take from this case:
-
Increased Oversight: Regulators are making Medicare Advantage a top compliance priority.
-
Individual Accountability: Executives, not just corporations, can face penalties.
-
Data Scrutiny: Risk adjustment submissions are under the microscope like never before.
-
Financial and Reputational Costs: Beyond fines, settlements erode trust and damage long-term business credibility.
A Pattern of Enforcement
This settlement is part of a larger trend. Over the past several years, multiple health plans have faced similar investigations and settlements over risk adjustment practices. For insurers, this suggests that auditing and compliance functions need to move from being a back-office formality to a boardroom priority.
“What we’re seeing is not isolated—it’s systemic. Enforcement is ramping up, and every plan should take notice.”
— Former Federal Prosecutor specializing in False Claims Act cases
Looking Ahead
The Freedom Health settlement is a stark reminder that the stakes in Medicare Advantage compliance are higher than ever. Insurers who proactively invest in robust compliance programs, accurate reporting, and transparent practices will not only avoid penalties but also position themselves as trustworthy partners in an increasingly skeptical regulatory environment.
The industry’s reputation, and the trust of beneficiaries, depends on it.
Sidebar: Settlements on the Rise
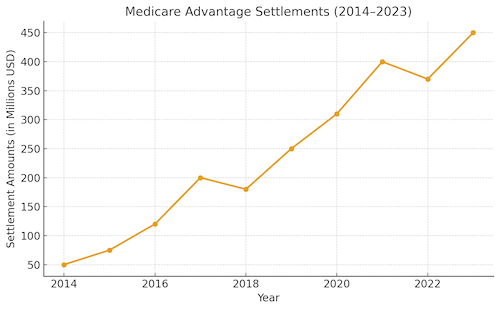
Over the past decade, Medicare Advantage settlements have steadily climbed, reflecting growing regulatory attention and enforcement actions.
Source: Industry analysis of False Claims Act enforcement