DOJ Sues California Medicaid Plan Over $320M Misused Federal Funds
 DOJ Lawsuit Against IEHP Spotlights Medicaid Compliance Challenges
DOJ Lawsuit Against IEHP Spotlights Medicaid Compliance Challenges
The insurance industry is no stranger to regulatory scrutiny, but the latest case against Inland Empire Health Plan (IEHP) is drawing fresh attention to how Medicaid funds are managed. The U.S. Department of Justice (DOJ) has filed a lawsuit alleging that IEHP, a California-based non-profit health plan, misused $320 million in surplus federal Medicaid funds.
These funds, allocated under the Affordable Care Act to expand Medi-Cal coverage, were intended to support patient care for newly eligible individuals. Instead, according to the DOJ, they were funneled toward unrelated expenses such as consulting contracts, technology services, and legal fees.
“Health plans entrusted with public funds must uphold the highest standards of compliance and accountability.”
– DOJ Complaint
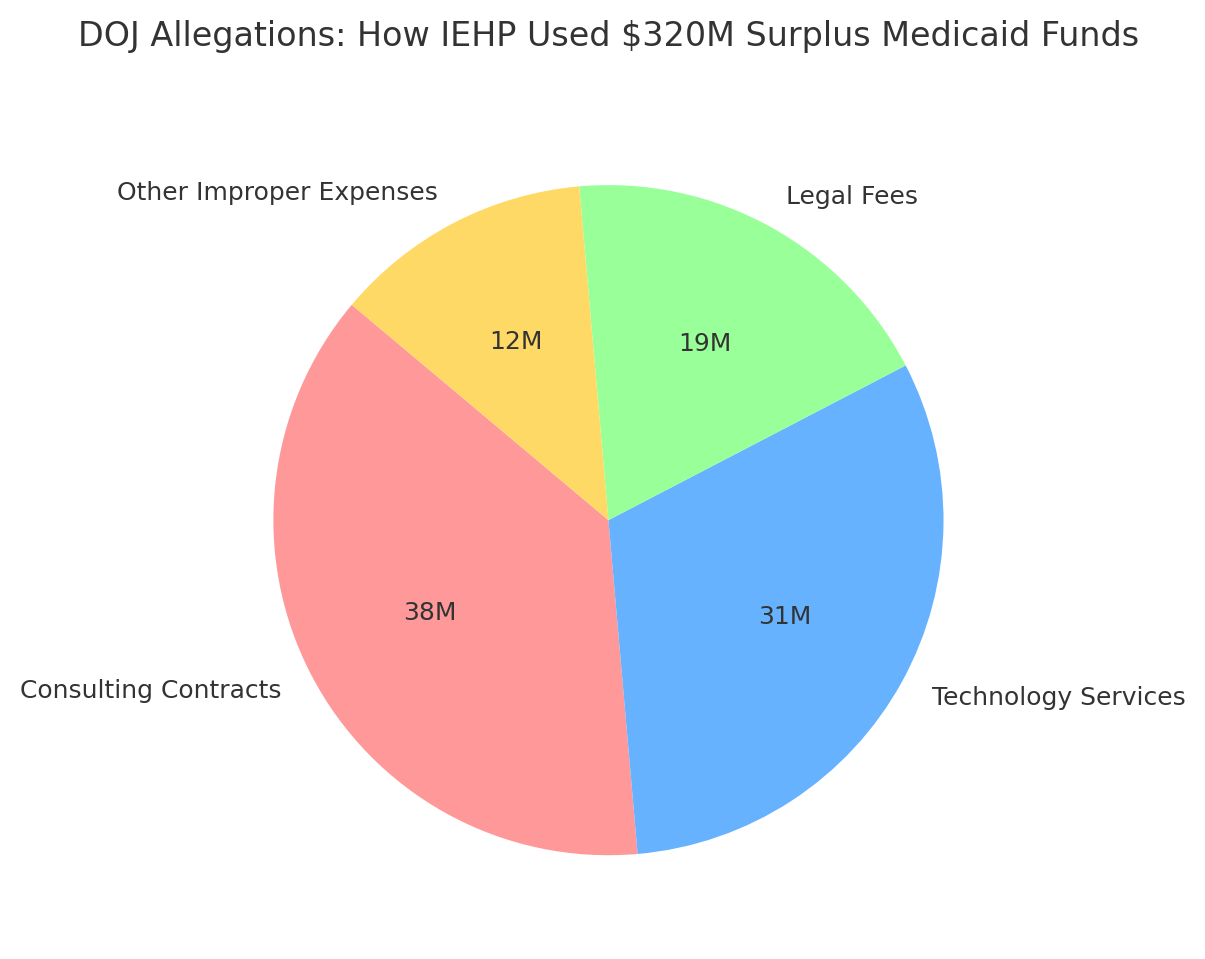
Breakdown of DOJ’s allegations on how IEHP redirected $320 million in surplus Medicaid funds.
Narrative:
The pie chart illustrates the DOJ’s claim that funds meant for patient care were instead funneled into consulting contracts, technology services, legal fees, and other non-medical expenses. While the exact figures are still subject to litigation, the overall message is clear: large sums of Medicaid dollars intended to support care for vulnerable populations were allegedly redirected away from their purpose.
What’s at Stake
At the heart of the lawsuit are accusations that IEHP violated the False Claims Act. The DOJ alleges the organization falsified expenditure reports and disguised payments to avoid returning surplus Medicaid dollars to state and federal authorities. Tactics cited include backdating expenses and rerouting payments through providers to make them look like incentive payments rather than improper costs.
This isn’t just a localized issue. The case underscores the national focus on Medicaid and Medicare fraud, an area where regulators have become increasingly aggressive. Previous cases have targeted schemes involving telemedicine, durable medical equipment, and even identity theft.
Why Compliance Matters for Insurers
For insurers operating in Medicaid markets, the implications are significant. Regulatory enforcement is becoming sharper, and the tolerance for financial misreporting is shrinking. Organizations must not only avoid wrongdoing but also actively prove that their compliance systems are airtight.
Here are a few key lessons insurers can take away from the IEHP case:
-
Transparency is non-negotiable: Funds must be accounted for clearly, with accurate reporting to state and federal regulators.
-
Surpluses are not discretionary: Any leftover Medicaid funds must be returned, not repurposed.
-
Internal controls are critical: Strong audit trails, oversight mechanisms, and independent compliance reviews help minimize risk.
-
Public trust is on the line: Mismanagement erodes confidence among patients, regulators, and partner organizations.
A Bigger Picture
The DOJ’s lawsuit is not only about reclaiming dollars but also about reinforcing the principle that Medicaid funds are meant for patient care, not discretionary spending. State-managed Medicaid entities play a critical role in ensuring that vulnerable populations receive coverage, and any misuse of funds threatens both patient outcomes and industry reputation.
“Compliance is not just a legal requirement, it’s the foundation of trust in public health coverage.”
– Health Policy Analyst
As managed care programs continue to grow in complexity, the industry should expect more audits, more lawsuits, and more accountability. For insurers, now is the time to double down on compliance frameworks that ensure funds are used as intended.