When Coverage Falls Short: A Shark Attack, a Prosthetic Hand, and a Bizzare Insurance Dilemma
In Virginia, a young mother is learning firsthand just how wide the gap can be between medical need and insurance coverage. After surviving a shark attack that took her arm, she is now facing another devastating blow: her insurer has denied coverage for the $73,000 advanced prosthetic hand she needs to regain daily independence.
This story has quickly become more than just a personal tragedy. It is a case study in how insurers and patients collide over the cost of emerging medical technologies, especially when those technologies fall into the gray area between "medically necessary" and "life-enhancing."
The Human Cost Behind the Numbers
A prosthetic hand is not simply a piece of equipment. For amputees, it is the bridge back to work, parenting, and normal life. Yet insurers often classify the most advanced prosthetics as “experimental” or “not medically necessary,” even when they are the only tools that allow a patient to regain a meaningful quality of life.
“They won’t help me,” said the Virginia mother in an interview after learning her insurer would not cover her prosthetic. “I just want to hold my child’s hand again.”
Stories like hers highlight how difficult it can be for patients to navigate insurance approvals after traumatic injuries. Insurers face growing pressure to contain costs, while patients and advocates argue that modern prosthetics should be considered as essential as other medical devices like pacemakers or wheelchairs.
Where Insurers Draw the Line
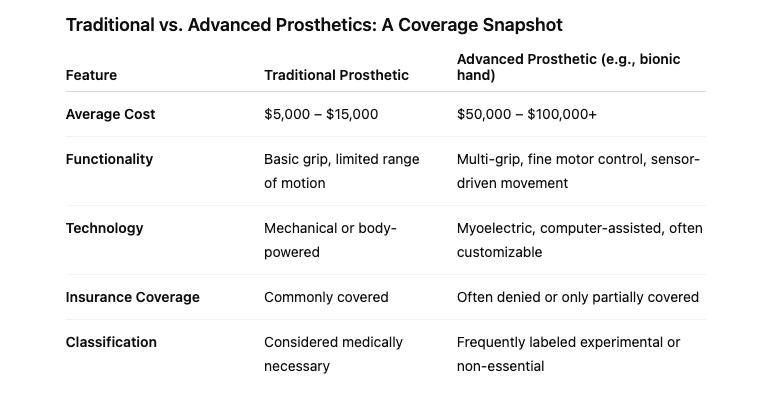
For carriers, high-tech prosthetics present a challenge. Advanced devices can cost anywhere from $50,000 to over $100,000. While traditional prosthetic limbs are typically covered, insurers often exclude advanced versions, citing their expense and lack of long-term clinical data.
Here are a few of the factors insurers commonly weigh:
-
Cost-benefit analysis: Is the prosthetic’s price justified by measurable patient outcomes?
-
Classification of medical necessity: Is the device required for basic function, or does it enhance function beyond “normal”?
-
Policy language: Many plans contain exclusions for “experimental” or “deluxe” devices.
-
Precedent in claims: Prior case outcomes influence approvals.
These questions leave room for interpretation, and it is patients like this Virginia mother who often get caught in the middle.
A System Under Pressure
The insurance industry is facing a new era in claims: rapid advances in medical devices are colliding with legacy coverage models. For insurers, the stakes are high. Expanding coverage for cutting-edge prosthetics could mean billions in additional costs, yet denying them invites public scrutiny and legal challenges.
“Every denied claim is a headline waiting to happen,” noted one healthcare analyst. “And when the human story is this powerful, insurers can’t afford to ignore the reputational risk.”
The industry is now asking itself whether prosthetics should be viewed as an extension of reconstructive care, or as a premium enhancement.
Looking Ahead
This case underscores the urgent need for clearer policy guidelines on advanced prosthetic coverage. As technology races forward, the insurance sector must grapple with balancing cost containment against public expectations of fairness and compassion.
For insurance professionals, the question is not just how to structure benefits today, but how to anticipate tomorrow’s advances. Whether it’s prosthetics, gene therapies, or AI-driven treatments, the same fundamental challenge will arise: where does “necessary care” end, and where does “enhanced living” begin?
“We don’t think about how often we use our hands to do tasks until you lose one,” said Foley.
A GoFundMe campaign has been launched to help Foley fund the bionic arm.