Billions on the Line: How Three Dropped Calls Sparked a Fight Over Medicare Star Ratings
When three phone calls failed at Humana’s customer service line, it set off a legal battle that could cost the health insurer billions. On the surface, it sounds absurd. But in the world of Medicare Advantage star ratings, every detail counts — right down to whether a call connects with an interpreter.
Why Star Ratings Matter
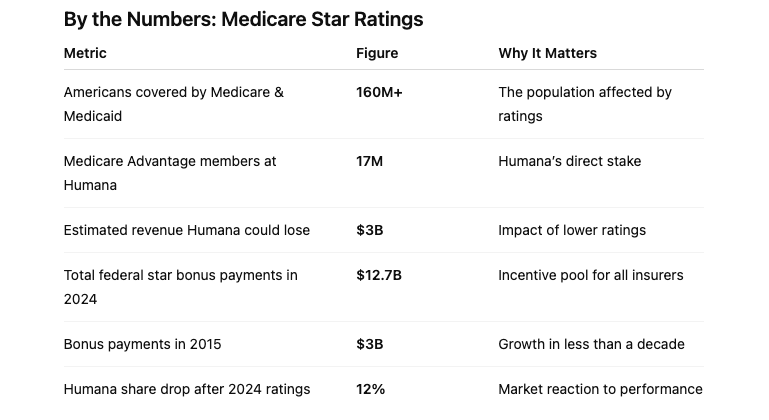
Star ratings, a product of the Affordable Care Act, score Medicare Advantage plans on a scale of one to five. They’re meant to help seniors and people with disabilities evaluate their coverage choices. In practice, though, the ratings are just as important to Wall Street as they are to patients.
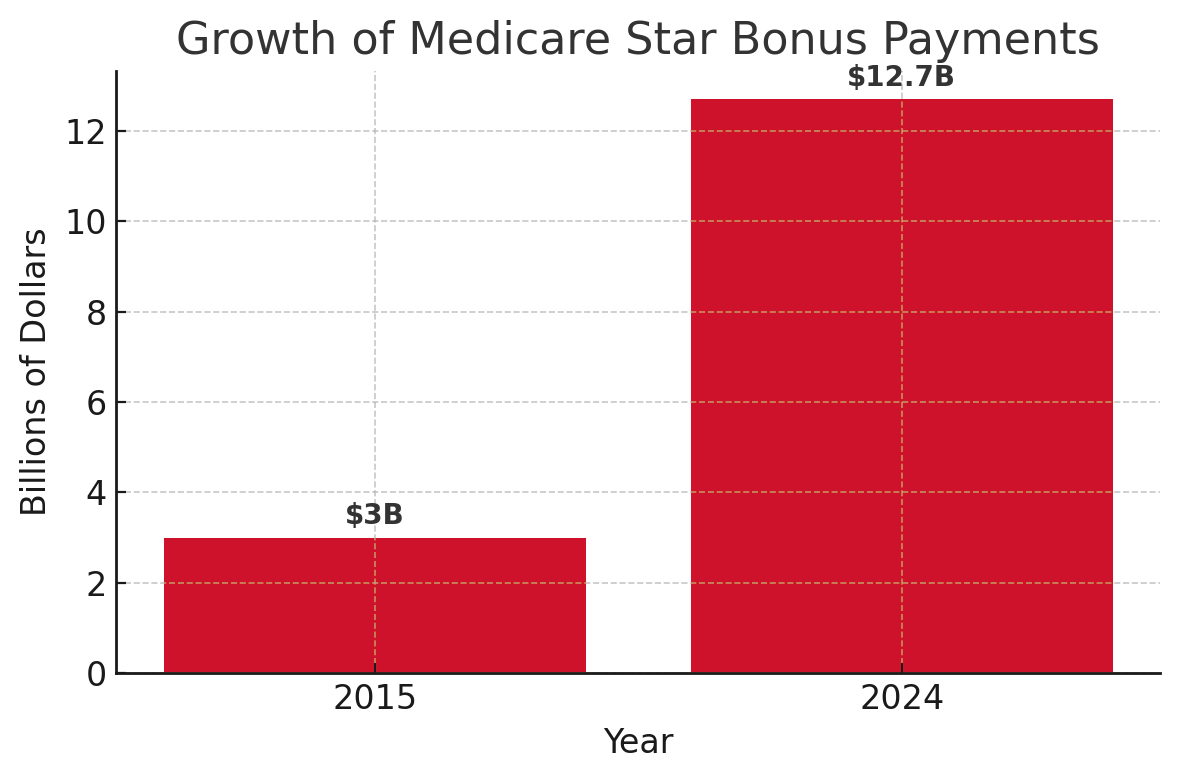
Plans with higher ratings attract bonus payments from the Centers for Medicare & Medicaid Services (CMS), allowing insurers to reinvest in richer benefits. In 2024 alone, those payments totaled nearly $13 billion, more than quadruple what the government spent in 2015.
“Star ratings play a more consequential role in the payments for insurers’ plans than they do in beneficiaries’ decisions about which plans to enroll in.”
— Jeannie Fuglesten Biniek, Associate Director, KFF
Humana, which covers roughly 17 million Americans, saw its stock tumble 12 percent last October after disappointing ratings. Analysts estimate that lower scores could cost the company $3 billion in lost revenue.
The Dispute at Hand
CMS requires a flawless record on foreign-language calls to earn top marks for call center performance. Humana failed three such test calls, allegedly hanging up on callers who needed interpreter assistance. The agency said the lapses reflected “shortcomings in providing the barest minimum of customer service.” Humana disagrees and is seeking a ruling before October 15.
This isn’t the first time ratings have hinged on dropped calls. UnitedHealth recently won its own court fight after a judge ordered CMS to recalculate ratings without penalizing a disputed call.
The Broader Industry Impact
The controversy highlights deeper questions about how much star ratings really reflect quality of care. With more insurers challenging CMS in court, the system itself is under scrutiny.
Some experts argue the system has grown overly complex, with dozens of metrics that may not always align with patient outcomes. For example, cancer screenings or chronic disease management arguably have more impact on health than call center logistics.
“It underscores the Byzantine nature of the star ratings system that you can have billions of dollars riding on whether a single call is dropped.”
— Matthew Gillmor, Director of Equity Research, KeyBanc
What’s Next for Insurers
The industry is bracing for CMS’s 2026 star ratings, due out in early October. With billions in bonus payments at stake, companies are leaving nothing to chance. The competition extends beyond compliance — it shapes how insurers market themselves and what benefits they can afford to offer.
Here’s what insurers are focusing on as they jockey for position:
-
Litigation strategies to challenge disputed CMS metrics
-
Operational fixes in call centers, especially for language access
-
Benefit design that leverages higher bonuses into richer offerings
-
Market positioning by emphasizing ratings in advertising and enrollment campaigns
Rethinking the Star System
Conservative policy groups like the Paragon Health Institute have gone as far as recommending elimination of the program, arguing that the link between ratings and true quality is tenuous. Others say reform, rather than removal, is the more practical path.
What’s clear is that insurers, regulators, and investors will continue to spar over what the ratings should measure and how they’re enforced. And for companies like Humana, the outcome of a few phone calls could determine billions of dollars in revenue — along with the benefits available to millions of Medicare members.