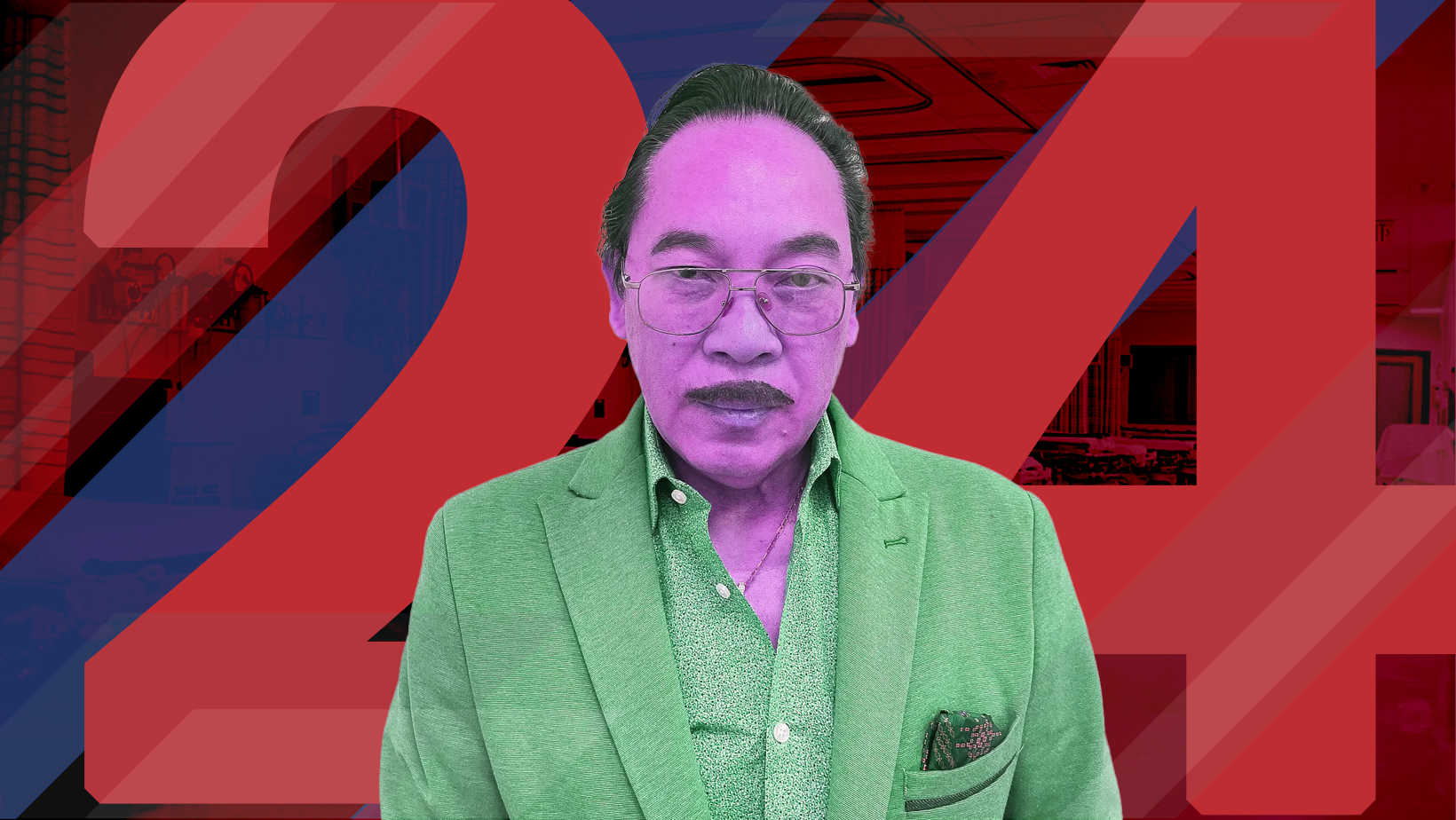
New York Doctor Sentenced for $24M Medicare Fraud Scheme Involving Kickbacks
A High-Profile Medicare Fraud Case Sends a Clear Signal to the Industry
The sentencing of Alexander Baldonado, M.D., a New York physician, is another stark reminder that Medicare fraud enforcement is not slowing down. Federal prosecutors secured a seven-year prison sentence after proving Baldonado orchestrated a sweeping fraud scheme that generated more than $24 million in Medicare claims tied to medically unnecessary services.
Beyond the prison term, Baldonado was ordered to pay more than $2.2 million in restitution, reflecting the portion of fraudulent claims that Medicare actually paid out. For insurers and compliance leaders, the case highlights familiar red flags that continue to attract intense regulatory scrutiny.
“This case demonstrates that healthcare fraud, especially when it exploits vulnerable Medicare beneficiaries, will be met with aggressive prosecution and serious consequences.”
Department of Justice, Criminal Division Fraud Section
How the Scheme Worked
According to trial evidence, Baldonado targeted Medicare beneficiaries who attended COVID-19 testing events. Without providing any medical treatment or meaningful consultations, he ordered high-cost cancer genetic tests and orthotic braces. Many patients never spoke with him at all.
In addition to unnecessary testing, Baldonado billed Medicare for office visits that never occurred. Investigators also documented illegal cash kickbacks paid to him by laboratories and a durable medical equipment supplier in exchange for signing off on orders.
Undercover footage introduced at trial showed Baldonado accepting bribes to approve prescriptions, reinforcing the government’s argument that the conduct was deliberate and systematic.
“The evidence showed hundreds of tests were authorized without medical justification, and in some cases, patients never even received their results.”
HHS Office of Inspector General
Why This Case Matters to Insurers
For payers, this case underscores the ongoing risk posed by providers who act as billing conduits rather than clinicians. The fraud relied on volume, speed, and the assumption that claims tied to COVID-related activity would face less scrutiny during a chaotic period.
Insurers should pay close attention to recurring indicators like:
-
Sudden spikes in high-cost genetic testing
-
Providers billing for services without corresponding clinical documentation
-
Unusual relationships between physicians, labs, and equipment suppliers
-
Claims tied to outreach events rather than established patient care
Part of a Broader Enforcement Push
Baldonado’s conviction did not happen in isolation. Federal authorities continue to roll out significant sentences across the country as part of the Health Care Fraud Strike Force Program. Recent cases include a Missouri man sentenced to 10 years for a cancer-related Medicare fraud scheme, a Michigan pharmacist convicted for billing for prescriptions that were never filled, and Arizona wound graft company owners sentenced in a case involving more than $1.2 billion in false claims.
Together, these cases reflect an enforcement environment that is increasingly coordinated and data-driven, with agencies sharing intelligence to identify patterns faster and intervene earlier.
“We are committed to protecting the integrity of Medicare and holding accountable those who abuse the system for personal gain.”
Federal Bureau of Investigation
What the Insurance Industry Should Take Away
The Baldonado case reinforces a reality insurers already understand: enforcement agencies are focused on medically unnecessary services, kickback arrangements, and schemes that exploit emerging healthcare trends. COVID-related programs may have created opportunity, but they also created data trails that investigators are now following aggressively.
For insurers, providers, and compliance professionals, this is a moment to reassess monitoring strategies, provider education, and fraud detection models. The penalties are severe, the investigations are deep, and the message from regulators is increasingly clear. Fraud in federal healthcare programs will be pursued, prosecuted, and punished.

