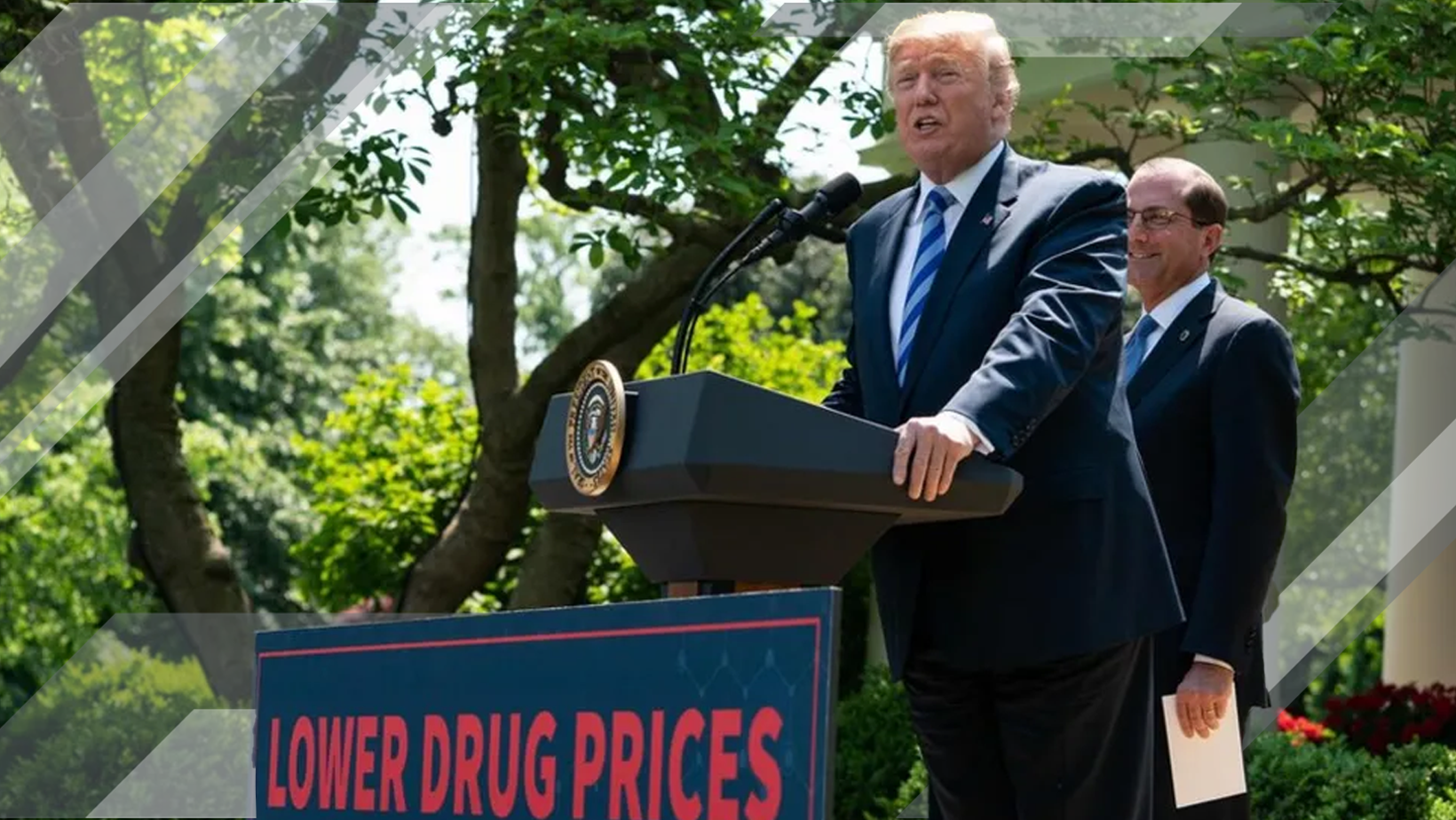
Trump Administration Secures Drug Price Reductions for Weight-Loss Meds in Medicare
Weight-Loss Drugs Get a Price Trim: What It Means for Insurers and the Future of Coverage
The Trump administration’s latest move to rein in prescription drug costs could shake up how insurers, employers, and consumers approach coverage for high-demand weight-loss medications. In newly announced agreements with Eli Lilly and Novo Nordisk, the administration set the stage for significant price cuts on leading drugs like Zepbound and Wegovy, with expanded Medicare access beginning in 2026.
A New Chapter in Drug Affordability
Starting in 2026, Medicare beneficiaries who meet certain body mass index (BMI) and health condition criteria—such as prediabetes, heart failure, or kidney disease—will be able to access these popular weight-loss drugs for a $50 monthly copay. Medicaid programs will have the option to join the initiative, potentially widening access even further.
These deals also include the creation of TrumpRx, a federal direct-to-consumer platform offering discounted medications. Oral versions of the GLP-1 drugs are slated to launch at $149 per month, a major drop from current retail prices that can exceed $1,000 monthly.
“We’re finally seeing a coordinated federal strategy to make breakthrough treatments affordable without sacrificing access,”
– Health Policy Analyst, Washington D.C.
Pricing and Market Impact
Under the new agreements, Medicare will negotiate average prices around $245 per monthly dose, while injectable options will range between $250 and $350, depending on dosage. For context, retail prices currently hover far above these levels, making affordability a central theme of the rollout.
The initiative aims to make these drugs available to about 10% of Medicare beneficiaries, a move expected to ripple through the broader insurance market. While employer-sponsored plans have slowly expanded their GLP-1 coverage, only 44% of large employers currently include these medications for weight management—a gap this policy could help narrow.
Key Takeaways for Insurers
The insurance sector is watching closely, as these developments could reshape benefit structures, premium calculations, and long-term claims forecasting.
-
Expanded Access: Medicare’s adoption of GLP-1 coverage may pressure private insurers to follow suit.
-
Cost Shifts: Lower negotiated prices could improve affordability but may also drive increased utilization.
-
Long-Term Savings: Better health outcomes among users could reduce downstream costs for chronic conditions.
-
Employer Impacts: With federal programs setting precedent, large group plans may reassess exclusions or tiering strategies.
Beyond Weight Loss: A Broader Strategy
This is not a one-off policy. The administration’s approach reflects a “most favored nation” pricing model, aligning U.S. drug prices with international benchmarks. Similar arrangements with Pfizer for Medicaid medications and EMD Serono for fertility treatments indicate a broader campaign to standardize affordability across therapeutic areas.
“We’re seeing a shift from piecemeal rebates to systemic pricing reform,”
– Pharmaceutical Market Research Director
For insurers, this shift could mean a recalibration of formulary management, pricing models, and provider negotiations—especially as more drugs enter the GLP-1 and metabolic therapy market.
Looking Ahead
While financial specifics remain in flux, early estimates suggest that improved health outcomes among treated populations could help offset new costs for Medicare and Medicaid. For the insurance industry, these developments underscore a growing intersection between public policy and private payer innovation.
As the line between government negotiation and market competition blurs, one thing is clear: the weight of drug pricing reform is finally being shared—and insurers will play a central role in how the benefits reach consumers.