Wellcare announces more Non Commissionable and Suppressed Plans for Plan Year 2026
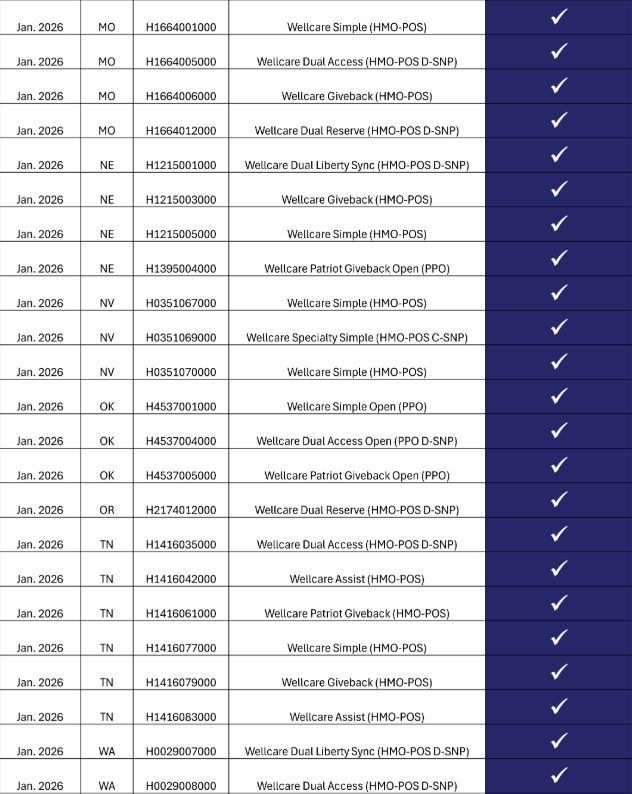
- 43 additional plans will be suppressed and non-commissionable in our vendor platforms for 2026 enrollment beginning Feb. 6, 2026. These plans will appear as quote only in the Ascend Enrollment Platform and will not be available for broker enrollment.
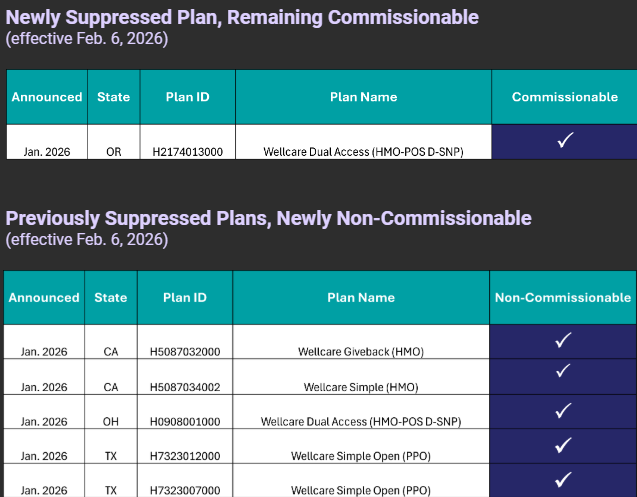
- One plan, Wellcare Dual Access in Oregon (H2174013000), will be suppressed beginning Feb. 6, 2026, but will remain commissionable.
- Five plans, previously suppressed for PY2026, will become non-commissionable beginning Feb. 6, 2026.
- Beneficiaries can self-enroll through Medicare.gov or by calling Wellcare for all plans.